Case Report
Hell J Surg. 2025 Jan-Mar;95(1):36–41
doi: 10.59869/25058
Konstantinos Bikas1,2, Nikolaos Chatziathanasiou1,2, Dimitrios Matsagkos2, Stavroula Papaeleftheriou2, Georgios Giannos2, Vasiliki Tseliou2, Athina Chrysikopoulou2, Stavroula Katsimente2, Aggeliki Koltsida2, Achileas Koulaxidis2, Georgios Taimpiris2, Teresa Bidetti2, Evangelos Velaoras2, Aikaterini Starka2, Marietta Lavrentaki2, Apostolos Sdrenias2, Nestor-Nikolaos Georgakakos2, Filalithis-Marios Mamakis2, Panagiotis Psychas2, Konstantina Sitouni1, Panagiotis Theodoropoulos2, Antonios Siakas2, Ioannis Tsiampas2, Hennadi Toka2, Georgios Floros2, Konstantinos Sfakianakis2, Nikolaos Kochylas2, Dimitrios Chasiotis2, Charalambos Kokkinos2, Georgios Papadopoulos2, Dimitrios Magganas2, Panagiotis Prigkouris2, Christos Kontovounisios2-5
1These two authors contributed equally to this work
22nd Surgical Department Evangelismos Athens General Hospital, Greece
3Department of Surgery and Cancer, Imperial College London, London, UK
4Department of General Surgery, Chelsea and Westminster Hospital, London, UK
5Department of Surgery, The Royal Marsden Hospital, London, UK
Correspondence: Christos Kontovounisios, Second Surgical Department Evangelismos Athens General Hospital, 45-47 Ipsilantou St., 106 76 Athens, Greece, e-mail: c.kontovounisios@hotmail.com
Abstract
Managing a short proximal colonic segment after an extensive left sided colon resection may be challenging. Total colectomy with ileorectal anastomosis (TC-IRA) is an option, but at the cost of sacrificing the whole colon and the ileocecal valve. Two organ- preserving alternatives are the Deloyers procedure (DP), which involves mobilisation and cranio-caudal rotation of the right colon around the axis of the ileocolic vessels and the retroileal trans-mesenteric method described by Turnbull. DP has been shown to be safe, with fewer postoperative bowel movements (average 3.5 with a median of 2-3 in DP versus average 4-6 with a median of 5 in TC-IRA) and equivalent anastomotic leak rates (<5%) compared with TC-IRA. Herein, we present a patient with a left colon adenocarcinoma, who was initially planned for a laparoscopic left hemicolectomy but intraoperatively converted to a laparoscopic assisted Deloyers procedure due to adverse intraoperative findings. This case highlights the feasibility of minimally invasive, assisted techniques in salvage settings and underscores the importance of colorectal surgeons being well-versed in this procedure, both open and laparoscopically, as it helps preserve colonic physiology and leads to improved functional outcomes.
Key Words: Case report, Deloyers, colon cancer, salvage, colonic inversion
Submission: 24.01.2025, Acceptance: 05.07.2025
Introduction
Performing extended left-sided colon resections and creating a tension-free anastomosis can be challenging, demanding both expertise and a thorough understanding of the anatomy. An extended left colectomy, whether planned preoperatively or determined intraoperatively, may leave the proximal colonic segment too short to reach the rectal stump without excessive tension, making the subsequent anastomosis risky [1]. Many surgeons therefore prefer to construct a total colectomy with ileorectal anastomosis (TC-IRA) [1]. This leads, however, to impaired bowel function, with persistent frequent bowel movements that negatively impact quality of life (QoL) over the long term [2].
Two traditional techniques are available to preserve the proximal colon while providing additional length to reduce tension in the anastomosis. The retroileal trans-mesenteric method, first described by Turnbull in 1978, involves creating a “window” in the terminal ileal mesentery and pulling the transverse colon through it into the pelvis [3]. The Deloyers procedure (DP), introduced in 1964, entails complete mobilisation of the right colon, which is then rotated 180 degrees counterclockwise around the axis of the ileocolic vessels to facilitate a colorectal or coloanal anastomosis [4]. Although these are old well described procedures, they were relatively abandoned in the past. In recent years however, they are used more frequently since conservation of as much gastrointestinal physiology as possible is thought to contribute to a better QoL. DP has been shown to be safe, with decreased postoperative bowel frequency and equivalent anastomotic leak rates compared with TC-IRA.
We report a case of a female patient with a left colon adenocarcinoma who was initially planned for a laparoscopic left hemicolectomy and was later converted to a laparoscopic assisted DP, due to unexpected intraoperative events.
This case highpoints the feasibility of minimal invasive assisted techniques in salvage procedures and highlights the importance of familiarity of colorectal surgeons with the DP, both open and laparoscopically, since it can restore the continuity of the gastrointestinal tract with a tension free anastomosis and with preservation of the ileocecal valve and colonic physiology.
Case presentation
A 71-year-old female patient, with a descending colon adenocarcinoma was admitted in our Surgical Department for surgical management.
One week prior to admission, she underwent a colonoscopy due to persistent anaemia. Near the hepatic flexure, it revealed a 3 cm sessile serrated lesion (SSL), occupying approximately 50% of the luminal diameter, which was subjected to endoscopic mucosal resection (EMR). At 50 cm from the anal verge, a 2 cm Paris IIa+c polyp was identified, biopsied and a tattoo was applied proximally. At 35 cm from the anal verge, a 1.5 cm Paris IIa polyp was observed and was biopsied. Histopathological examination of the Paris IIa+c polyp confirmed the presence of moderately differentiated adenocarcinoma. Both the 3cm SSL and the1.5 cm Paris IIa polyp were benign adenomas.
Upon her admission, she underwent a thorough physical and pre-operative work up. Her medical history consisted of mild idiopathic hypertension, controlled with nifedipine, dyslipidaemia and obesity with a basal metabolic index (BMI) of 34. She had two natural births at the age of 29 and 31 and she had undergone an open appendectomy more than 20 years ago. She had never smoked and she was a social drinker. Her family history was insignificant with no cancer prevalence among first degree relatives. On clinical examination, her abdomen was soft, non-tender with no identifiable masses and digital rectal examination did not reveal any pathology. The remainder of the physical assessment was unremarkable. Tumour markers CEA, CA 19-9, CA125 and CA15-3 were within normal values.
On the second day of her admission, abdominal and chest contrast-enhanced computed tomography (CT) imaging were obtained and did not reveal any lymphadenopathy or distant metastases. On the next day, the case was presented to the multidisciplinary team (MDT) and a laparoscopic left sided colon resection was decided
The following day, the patient was transferred to the operation theater and positioned in a modified lithotomy position. A supraumbilical camera port was inserted via the Hasson open technique. Pneumoperitoneum of 14mmHg pressure was established and additional laparoscopic ports were placed; 5 mm in the left iliac fossa, 12 mm in the right iliac fossa, and 5 mm in the right upper quadrant. Initial laparoscopy revealed no peritoneal metastases or other suspicious lesions. The site of a previous appendectomy was noted, along with dense adhesions between the omentum, the left colon and the spleen. Adhesiolysis was performed and a tattoo marking at the junction of the sigmoid/ descending colon was visualised. The inferior mesenteric artery (IMA) pedicle was identified, and a surgical plane was developed between the posterior peritoneum and the Gerota’s fascia. The left ureter and ovarian vessels were identified and preserved. The dissection continued along the previous plane and the IMA was clipped and divided at its origin. A distinct inferior mesenteric vein was not visualised. During lateral mobilisation, detachment of the transverse colon from the spleen revealed a second tattoo, which was not mentioned in the pre-operative colonoscopy report. It was sited proximal to the splenic flexure, requiring an extended left hemicolectomy. Transverse colon was further mobilised, and the middle colic vessels were clipped and divided. The transverse mesocolon was detached from the pancreas, the site of division was marked and the colon was transected with a linear stapler, just distal to the hepatic flexure. Due to the short length of the remaining transverse colon and the anticipated tension on the future anastomosis, a salvage Deloyers procedure was scheduled. Further mobilisation of the caecum and the right colon was performed. The mesocolon was transected near the bowel with division of the right colic vessels, while preserving arterial supply through the marginal artery and the ileocolic vessels.
At this stage, the surgical team was notified by the anaesthesiologist that there were ventilation issues and high blood carbon dioxide (CO2) levels. After a failed trial of lowering pneumoperitoneum pressure to 10mmHg and avoiding steep Trendelenburg position, the rest of the procedure was converted to open. A midline supra- and infraumbilical incision was performed, the specimen was delivered through the incision and resection was completed with distal transection at the level of the upper rectum, using a circular stapler. Using the ileocolic vessels as an axis, the colon was inverted caudo-cranially by 180 degrees in the sagittal plane, thereby repositioning the caecum to a subhepatic location and the transverse colon into the pelvis (Figures 1, 2). A tension-free end-to-end isoperistaltic anastomosis was constructed using a 28 mm circular stapler, reinforcing it with interrupted sutures. Airleak test was negative. A defunctioning stoma was deemed unnecessary. Meticulous haemostasis was ensured and mesenteric defects were closed. The peritoneal cavity was irrigated and a closed suction drain was placed in the pelvis. Abdominal wall closure was performed and the patient was extubated and recovered uneventfully. The length of the operation was approximately 240 minutes.
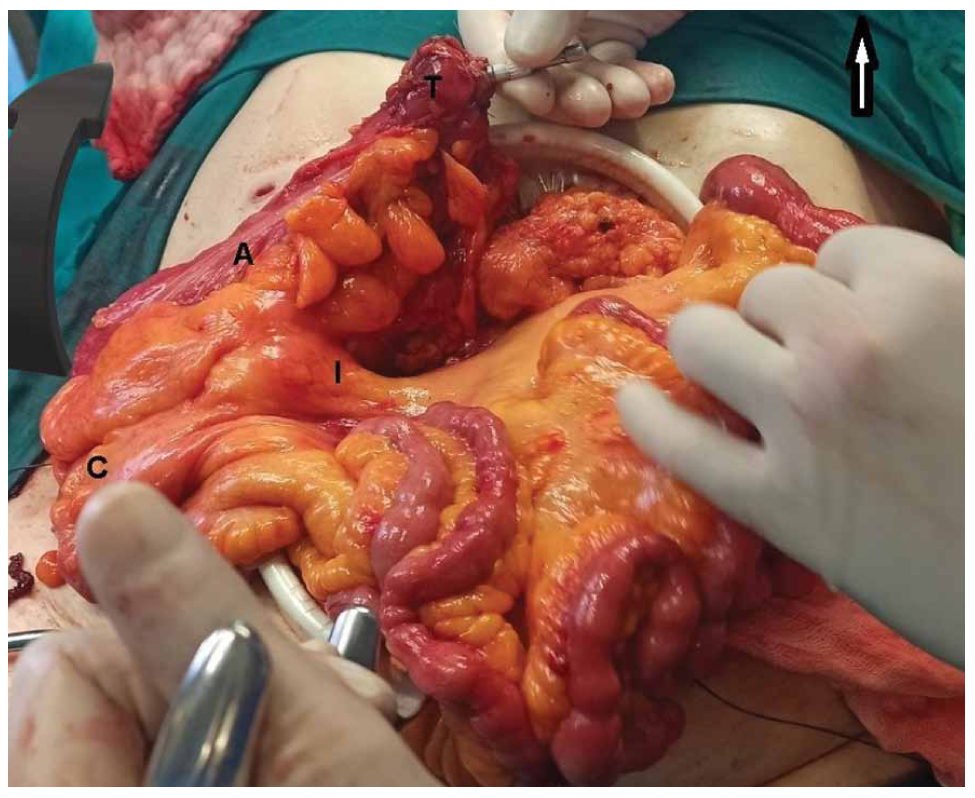
Figure 1. Intraoperative view of the proximal colon prior to inversion. Arrow at the upper left corner pointing towards the patient’s head. Curved black arrow showing the direction of caudo-cranial inversion A, anterior surface of the proximal colon; C, caecum; T, cut end of the transverse colon; I, ileocolic pedicle.
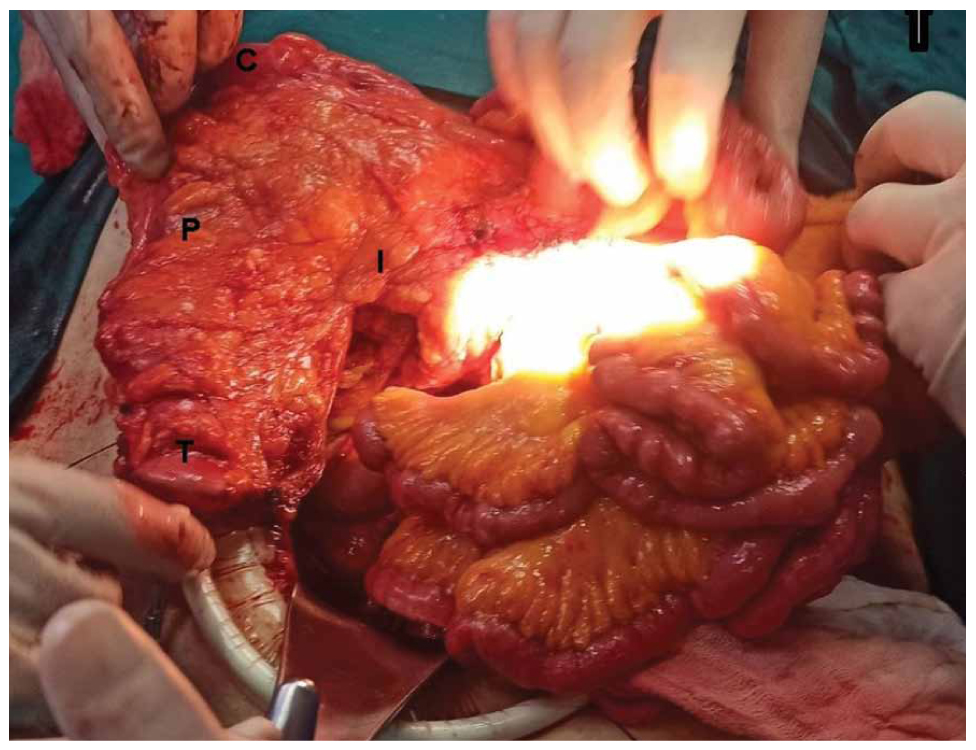
Figure 2. Intraoperative view of the proximal colon after inversion. Arrow at the upper left corner pointing towards the patient’s head; P, posterior surface of the proximal colon; C, ceacum; T, cut end of the transverse colon; I, ileocolic pedicle.
Post-operative course was uneventful, with no signs of anastomotic leak or any other complication. Diet commenced early on the second postoperative day and advanced gradually as tolerated. The drain was removed on the seventh and the patient was discharged on the eighth postoperative day.
Histopathology report showed a pT3N1 moderately differentiated adenocarcinoma of the colon, which corresponded to the more proximal tattoo in the transverse colon. Neoplastic cells were found to infiltrate the full thickness of the colonic wall and extend into the pericolic adipose tissue. There was also evidence of perineural and perivascular invasion, along with vascular emboli containing neoplastic cells. Neoplastic involvement was noted in one of the eighteen (1/18) regional lymph nodes harvested. Resection margins were negative. The tumour demonstrated positive immunohistochemical staining for MSH2, MLH1, PMS2, and BRAFV600E, suggesting proficient mismatch repair mechanisms (pMMR).The distal tattoo that was initially recognised at the junction of the descending/sigmoid colon, corresponded to the 1.5 Paris IIa polyp, which was a benign adenoma. With the biopsy results, the case was re-presented at the MDT meeting and a plan for adjuvant therapy was decided in six to eight weeks after the procedure.
The patient was subsequently re-evaluated at one and six weeks postoperatively before the commencement of the adjuvant chemotherapy. Clinically, she demonstrated a favorable recovery profile, having resumed a standard diet and gained 3 kilograms. Her bowel movements progressively stabilised, returning to a physiological pattern of less than two per day.
Discussion
Initially reported in 1958, colonic derotation, commonly referred to as the Deloyers procedure (DP), has been widely employed to maintain colon length following extensive colonic resections for various conditions both benign and malignant (Table 1).
This procedure entails the complete mobilisation of the right colon, transection of the middle colic and frequently the right colic vessels, appendicectomy and a 180-degree counter-clockwise colonic rotation in the coronal plane, allowing for a tension-free colorectal or coloanal anastomosis while maintaining adequate perfusion from the ileocolic vessels [4,6]. To preserve bowel function after surgery, the ascending colon is kept as long as possible, with careful attention given to ensuring adequate perfusion of the distal anastomosis, by preserving the marginal artery and the ileocolic pedicle [7]. A modification of this technique, described by Kontovounisios et al., involves a 180-degree craniocaudal inversion in the sagittal instead of the coronal plane, around the axis of the ileocolic vessels, with or without transection of the right colic vessels [8]. In addition to the traditional open approach, the DP has been successfully performed both laparoscopically and robotically.
With respect to the functional outcomes of open DP, two studies demonstrated that the majority of patients experienced a bowel movement (BM) frequency of approximately three times per day; mean 3.5 [19] and median 3 [13], respectively. In a smaller study by Kontovounisios et al., using the modified DP, patients had a median of 2 BM per day [8] (Table 2).
The anastomotic leak (AL) rate in DP with colorectal anastomosis has been reported to be low, but the absence of large-scale studies limits the ability to draw definitive conclusions. In two cohort studies, leak rate was 0% [8,13], whereas a recent study of 97 patients undergoing DP found AL in 5 patients (~5%) [16] (Table 2). With coloanal anastomosis, the risk of anastomotic complications is expected to be higher [17,20]; assessing blood flow to the residual colon and the anastomosis is therefore crucial. Intraoperative indocyanine green (ICG) fluorescence imaging has been found to be a valuable modality for accessing the perfusion in left-sided resections [18]. Late complications of the Deloyers technique include anastomotic stricture and chronic leak, with a reported incidence of 6% and 2% respectively [16].
Comparison between the DP, TC-IRA, and the retroileal trans-mesenteric Turnbull procedure is limited by the absence of large-scale, comparative studies. For the Turnbull technique, with the exception of an old study by Nafe et al. in 1994, which showed an AL rate of 3% [21], no major studies detail functional outcomes or complication rates [22]. A small retrospective study, comparing it with the DP, found no significant differences in the complication rate, including the AL [22].
Respective data for the TC-IRA are predominantly derived from cohorts with ulcerative colitis, necessitating cautious interpretation. Following this procedure, data from a review article report a bowel frequency of around 4–6 movements/day [23], while a recent study found a median of 5 BM daily [24]; numbers are slightly higher than the respective data observed post-DP (Table 2).Another study, with small sample sizes but not involving patients with ulcerative colitis, found a median of 3.5 BM daily after TC-IRA for colonic cancer, but decreased frequency (median 2.5 movements/ day) if the underlying pathology was diverticular disease or chronic slow transitconstipation with megacolon [2]. AL rates seem to be comparable: a systematic review across 15 studies reported a leak rate of 3.9% after a TC-IRA [25], while another, encompassing five studies, found rates ranging from 1.6% to 5.4% [26]. Analogously, in DP, reported leak rates vary from 0% to ~5% (Table 2). Fewer BM in DP and an equivalent AL rate were also observed in a small comparable study by Carpinteyro-Espin et al. [27].
Conclusion
Restoring continuity after extended left colon resections can be particularly challenging. Classically a total colectomy with ileorectal anastomosis (TC-IRA) is performed. Two main alternative techniques have been described that preserve the proximal colon; the retroileal trans-mesenteric method described by Turnbull and the Deloyers procedure that involves a complete mobilisation and rotation of the proximal colon and a colorectal or coloanal anastomosis. Its main advantages are that it spares the ileocecal valve and preserves large bowel length with possibly better functional outcomes compared to an ileorectal anastomosis after a TC-IRA. Leak rates are reported to be low and it has been employed in a variety of clinical situations both for benign and malignant diseases whether planned preoperatively or decided intraoperatively as a salvage procedure, as in our case.
Despite being performed for over six decades, robust, high-quality data on the surgical and functional outcomes of this procedure remain limited. Well-designed large-scale cohort and comparative studies are essential to generate high-level evidence regarding both the procedure itself and its comparison with alternatives such as the Turnbull procedure or the TC-IRA.
References
- Seow-En I, Ke TW, Chang SC, Chen WT. Laparoscopic retrojejunal trans-mesenteric anastomosis for extended left-sided colorectal resections – a new solution to an old problem. Colorectal Dis. 2021 May;23(5):1262-7.
- Lim JF, Ho YH. Total colectomy with ileorectal anastomosis leads to appreciable loss in quality of life irrespective of primary diagnosis. Tech Coloproctol. 2001 Aug;5(2):79-83.
- Rombeau JL, Collins JP, Turnbull RB, Jr. Left-sided colectomy with retroileal colorectal anastomosis. Arch Surg. (Chicago, Ill: 1960). 1978 Aug;113(8):1004-5.
- Deloyers L. Suspension of the Right Colon Permits Without Exception Preservation of the Anal Sphincter After Extensive Colectomy of the Transverse and Left Colon (Including Rectum). Technic -Indications- Immediate And Late Results. Lyon Chirurgical. 1964;60:404-13.
- Elhalaby I, Lim IIP, Bokova E, Egbuchulem IK, Rentea RM. Colonic Derotation Revisited: The «Deloyers Procedure» for Long-Segment Hirschsprung Disease. Cureus. 2024 Dec;16(12):e75539
- Jouvin I, Pocard M, Najah H. Deloyers procedure. Journal of visceral surgery. 2018;155(6):493-501.
- Okamoto K, Emoto S, Sasaki K, Nozawa H, Kawai K, Murono K, et al. Extended left colectomy with coloanal anastomosis by indocyanine green-guided deloyers procedure: A Case Report. J Anus Rectum Colon. 2021 Apr;5(2):202-6.
- Kontovounisios C, Baloyiannis Y, Kinross J, Tan E, Rasheed S, Tekkis P. Modified right colon inversion technique as a salvage procedure for colorectal or coloanal anastomosis. Colorectal Dis. 2014 Dec;16(12):971-5.
- Antona AD, Reggio S, Pirozzi F, Corcione F. Laparoscopic 3D high-definition Deloyers procedure: When, how, why? Updates Surg. 2016 Mar;68(1):111-3.
- Sciuto A, Grifasi C, Pirozzi F, Leon P, Pirozzi RE, Corcione F. Laparoscopic Deloyers procedure for tension-free anastomosis after extended left colectomy: Technique and results. Tech Coloproctol. 2016 Dec;20(12):865-9.
- Otani K, Nozawa H, Kiyomatsu T, Kawai K, Hata K, Tanaka T, et al. Laparoscopic Deloyers procedure to facilitate primary anastomosis after extended resection for synchronous cancers of transverse colon and rectum: Easy to preform with good functional outcome. Tech Coloproctol. 2017 Nov;21(12):975-6.
- Costalat G, Garrigues JM, Didelot JM, Yousfi A, Boccasanta P. Subtotal colectomy with ceco-rectal anastomosis (Deloyers) for severe idiopathic constipation: an alternative to total colectomy reducing risks of digestive sequelae. Ann Chir. 1997;51(3):248-55.
- Manceau G, Karoui M, Breton S, Blanchet AS, Rousseau G, Savier E, et al. Right colon to rectal anastomosis (Deloyers procedure) as a salvage technique for low colorectal or coloanal anastomosis: postoperative and long-term outcomes. Dis Colon Rectum. 2012 Mar;55(3):363-8.
- Dux J, Katz E, Adileh M, Segev L, Hazzan D. Restoring intestinal continuity in a hostile abdomen: The Deloyers Procedure. JSLS. 2021 Apr-Jun;25(2):e2021.00004.
- Ceylan C. Firearm injury and the Deloyers procedure: Case report and literature review. Ulus Travma Acil Cerrahi Derg. 2024 Apr;30(4):305-8.
- Sobrado LF, Schabl L, Foley NM, Prien C, Nahas SC, Liska D, et al. Deloyers technique for restoration of bowel continuity following extended left hemicolectomy: A Comprehensive Analysis of 97 Cases and Literature Review. Dis Colon Rectum. 2025 Apr 1;68(4):466-74.
- Ellis CT, Maykel JA. Defining anastomotic leak and the clinical relevance of leaks. Clin Colon Rectal Surg. 2021 Oct;34(6):359–65
- Morales-Conde S, Alarcón I, Yang T, Licardie E, Camacho V, Aguilar Del Castillo F, et al. Fluorescence angiography with indocyanine green (ICG) to evaluate anastomosis in colorectal surgery: Where does it have more value? Surg Endosc. 2020 Sep;34(9):3897-907.
- Sobrado LF, Schabl L, Foley NM, Prien C, Nahas SC, Liska D, et al. Deloyers technique for restoration of bowel continuity following extended left hemicolectomy: A Comprehensive Analysis of 97 Cases and Literature Review. Dis Colon Rectum. 2025 Apr;68(4):466-74.
- Platell C, Barwood N, Dorfmann G, Makin G. The incidence of anastomotic leaks in patients undergoing colorectal surgery. Colorectal Dis. 2007 Jan;9(1):71-9.
- Nafe M, Athanasiadis S, Köhler A. Indications and technique of retro-ileal colorectal anastomosis after expanded left-sided hemicolectomy. Chirurg. 1994 Sep;65(9):804-6.
- Dalmau M, Marti-Gallostra M, Pellino G, Espin-Basany E, Armengol M. The colon does not reach! A technical note with tricks to avoid colorectal anastomoses under tension. Colorectal Dis. 2024 Mar;26(3):564-9.
- da Luz Moreira A, Lavery IC. Ileorectal anastomosis and proctocolectomy with end ileostomy for ulcerative colitis. Clin Colon Rectal Surg. 2010 Dec;23(4):269-73
- Abdalla M, Norblad R, Olsson M, Landerholm K, Andersson P, Söderholm JD, et al. Anorectal function after ileo-rectal anastomosis is better than pelvic pouch in selected ulcerative colitis patients. Dig Dis Sci. 2020 Jan;65(1):250-9.
- Al-Rashedy M, Mukherjee T, Askari A, Gurjar S. A systematic review of outcomes and quality of life after ileorectal anastomosis for ulcerative colitis. Arab J Gastroenterol. 2023 May;24(2):79-84.
- Orchard MR, Saracino A, Hooper J, Shabbir J. Ileorectal anastomosis in ulcerative colitis: what do surgeons and patients need to know? A systematic literature review. Ann R Coll Surg Engl. 2025 Mar;107(3):174-9.
- Carpinteyro-Espín P, Santes O, Moctezuma-Velazquez P, Navarro-Iñiguez JA, Navarro-Navarro A, Salgado-Nesme N. Deloyers procedure compared to ileorectal anastomosis as restoration techniques of bowel continuity after extended left colon resection. ANZ journal of surgery. 2023;93(4):956-62.
- Zornoza M, Muñoz L, Ruiz A, De la Torre L. Surgical maneuvers for long-segment Hirschsprung pull-through in unique patients. Pediatr Surg Int. 2024 Jul;40(1):180.