Case Report
Hell J Surg. 2025 Jan-Mar;95(1):42–45
doi: 10.59869/25059
Athanasios Kontos1, Ioannis I. Tziortziotis1, Dimitrios Kypraios1, Maria Arnaouti2, Dimitrios Dimitroulopoulos1
1Gastroenterology Department of Cancer Hospital “Agios Savvas”, Greece
2Pathology Department of Cancer Hospital “Agios Savvas”, Greece
Correspondence: Athanasios Kontos, Gastroenterology Department of Cancer Hospital “Agios Savvas”, Alexandras av. 171, 11522, Athens, Greece, e-mail: athdkontos@gmail.com
Abstract
Many patients are diagnosed with pancreatic lesions nowadays. The differential diagnosis of pancreatic lesions is broad, including both benign and malignant causes. Endoscopic ultrasound (EUS) is a useful diagnostic tool for investigating such lesions, as it offers the advantage of obtaining specimens for histological examination. Here, we present a case of a patient with the rare diagnosis of pancreatic tuberculosis.
Key Words: Pancreas, tumor, tuberculosis
Submission: 02.05.23, Acceptance: 10.07.2023
Introduction
The pancreas is a common site of different and various lesions. These lesions can be benign such as IPMN (Intraductal Papillary Mucinous Neoplasm), autoimmune pancreatitis, infections, and others, or malignant, such as adenocarcinoma, neuroendocrine carcinomas etc [1-2]. The most common causes of infection are viruses (CMV, HSV, coxsackie virus, VZV, HIV), bacteria (Legionella, Leptospira, Salmonella, Mycoplasma, Brucella, Salmonella Typhi), fungi (Aspergillus), parasites (Toxoplasma, Cryptosporidium, Ascaris lumbricoides) [1-2].
In some cases, benign pancreatic tumors can mimic pancreatic cancer, and the diagnosis can only be made by obtaining a specimen from the lesion via endoscopic ultrasound (EUS) [2]. Pancreatic lesions are now better understood and more frequently and accurately diagnosed due to Computed Tomography (CT) and Endoscopic Ultrasound (EUS) which provides the ability to take biopsies through Fine Needle Biopsy (FNB) [2-3].
This case report presents a rare case of a pancreatic tumor, with a non-specific clinical presentation, which was revealed after EUS-FNB to be an unexpected and favorable benign outcome, of pancreatic tuberculosis.
Case Presentation
A 68-year-old male patient with a medical history of hypertension and dyslipidemia, with no history of immunosuppression or past tuberculosis infection or suspicious travels presented to our endoscopic department to investigate a pancreatic tumor that was found on a Computed Tomography (CT) scan. The initial evaluation of the patient and the prescription of the CT imaging was made by the GP. The symptoms that lead the patient to the GP were fatigue, weight loss (10kg the last 3 months) and mild abdominal pain. The clinical examination revealed stable vital signs and abdominal examination was unremarkable. His complete blood counts, liver function, renal function and coagulation profile were within normal limits. Inflammation markers, such as CRP and ESR, were elevated and specifically 10.90 mg/dl (Normal Values: 0-3mg/dl) and 35mm/hr (Normal values: 0-15mm/hr) respectively. Tumor markers, such as CEA, PSA, and AFP, were unremarkable except for a mild elevation of Ca19-9 which was 44,6 U/mL (Normal values: 0-37U/ml).
The CT that he brought showed a mass lesion in the head of the pancreas (Figure 1A, 1B) measuring 4.0 x 4.5 x 4.1 cm. No other imaging tests have been performed. The EUS revealed a hypoechogenic compact mass with homogeneous texture and longest diameter approximately 4cm, which did not infiltrate the main pancreatic duct, the common bile duct or important blood vessels. The extra-hepatic bile tree was normal. There were no lymph nodes near the pancreas or hepatic lesions that were suspected of metastasis (at the region that we could examine). EUS-FNB performed through the stomach, with a 22-gauge needle, was performed. Pathology test revealed a rare diagnosis and particularly: necrotic granulomatous inflammation, composed of central necrotic zone surrounded by epithelioid histiocytes with varied numbers of multinucleated giant cells and lymphocytes (Figure 2 and 3). Finally, Ziehl-Neelsen staining revealed the diagnosis of pancreatic tuberculosis (Figure 4A, 4B).
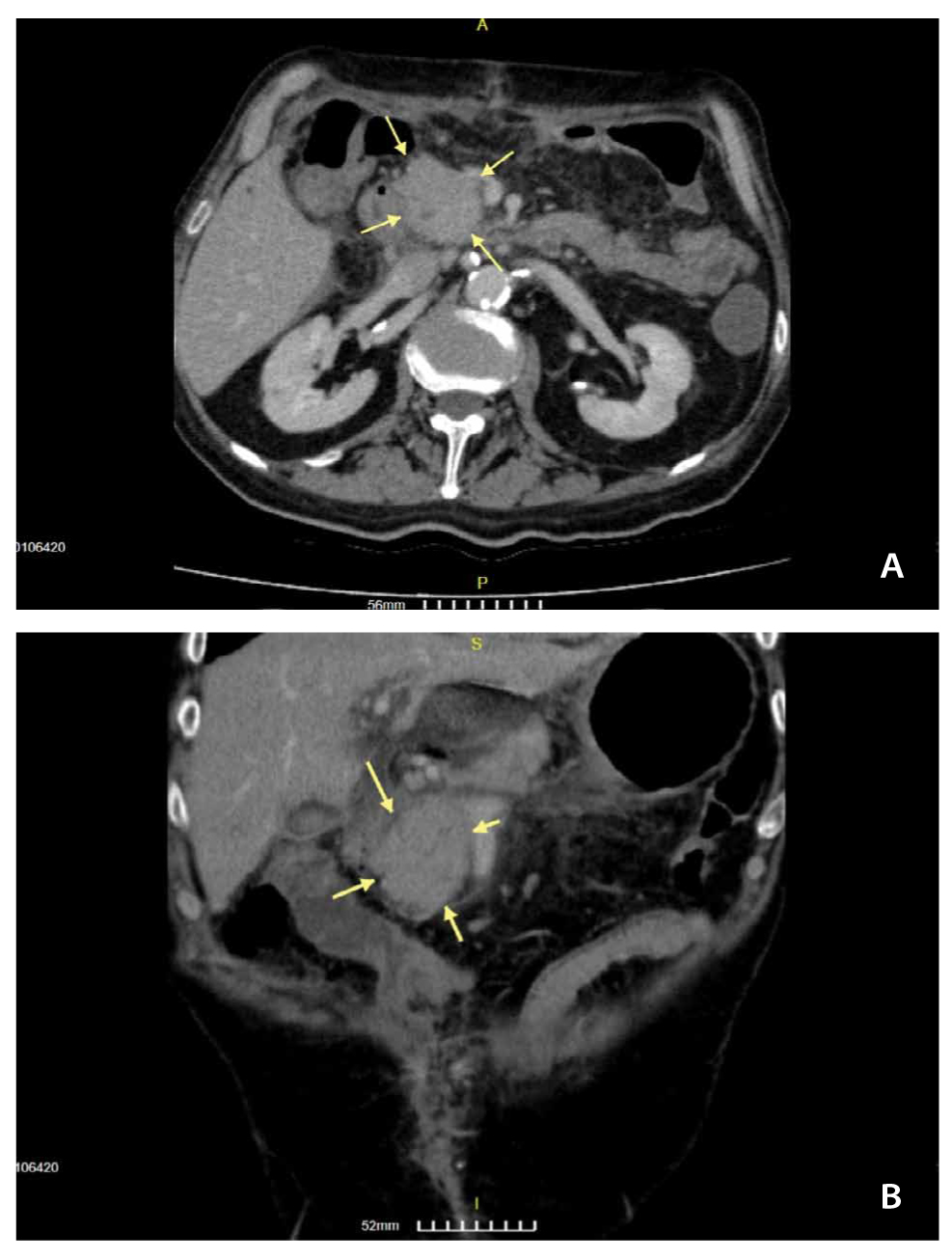
Figure 1. A – B. The yellow arrows show the pancreatic tumor that led the patient to EUS-FNB for the final diagnosis.
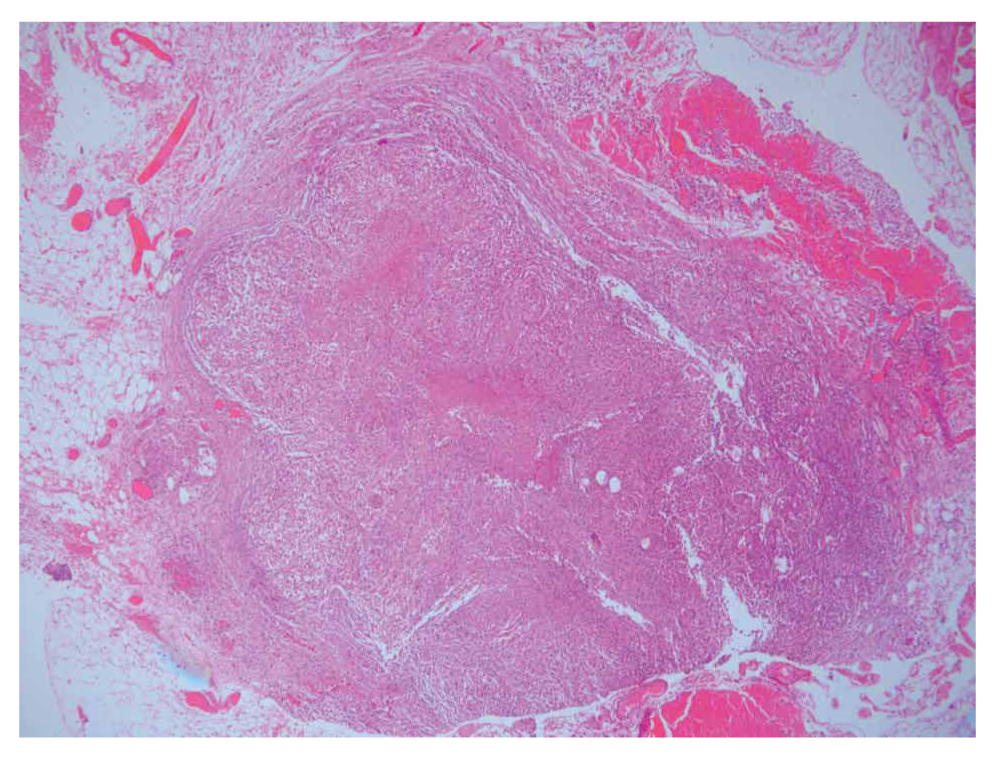
Figure 2. Central zone of necrosis.
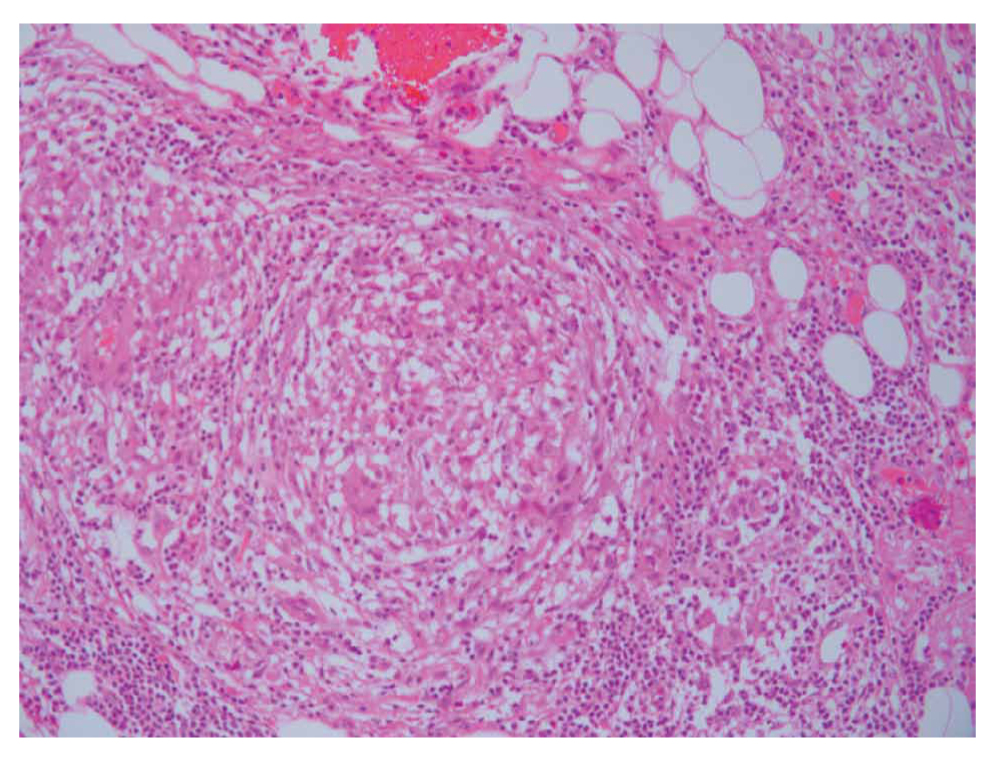
Figure 3. Epithelioid histiocytes with multinucleated giant cells and lymphocytes.
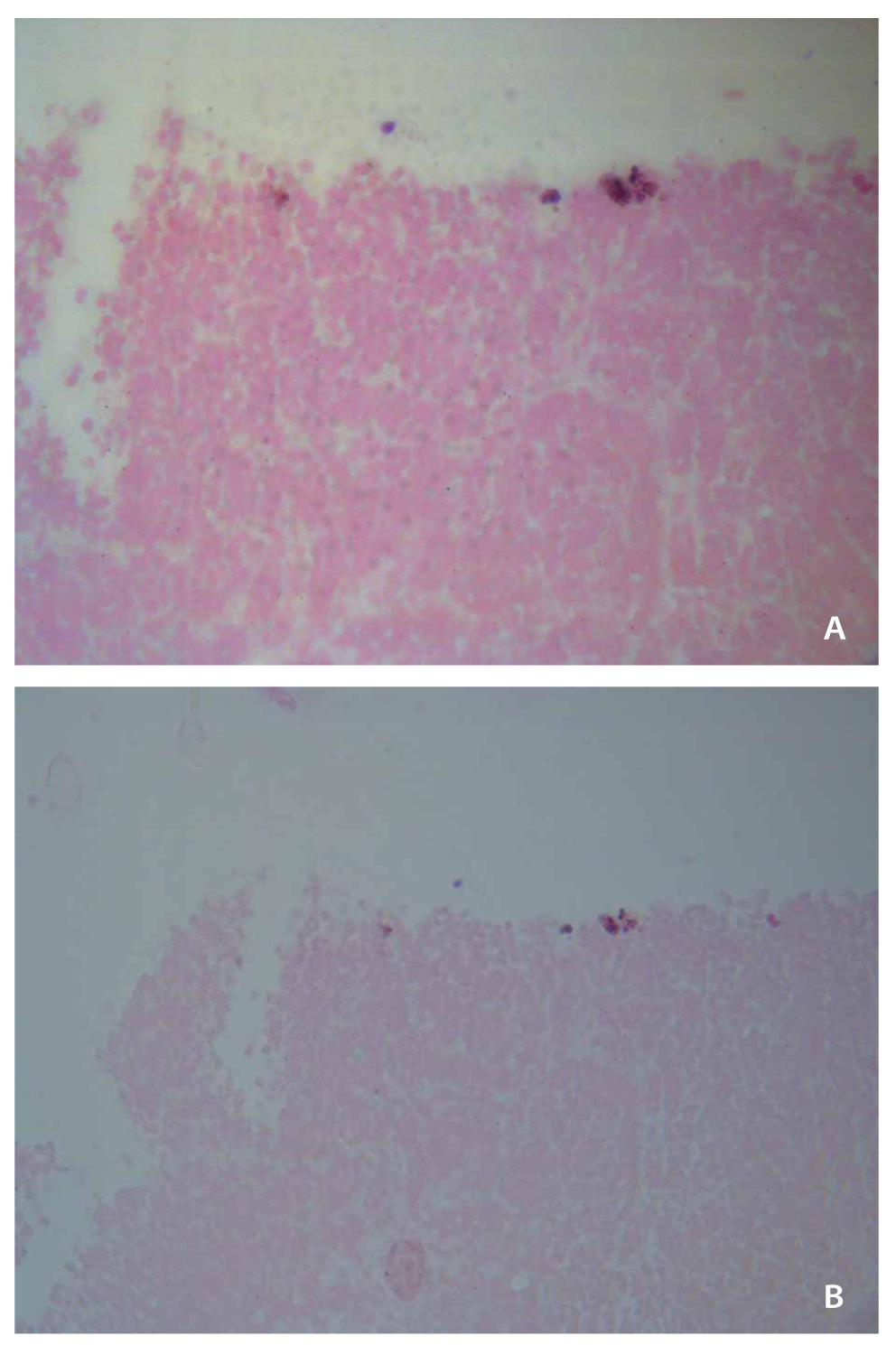
Figure 4. A – B. Ziehl-Neelsen stain for Mycobacteria Tuberculosis.
Discussion
Tuberculosis (TB) is caused by Mycobacterium Tuberculosis. Most of Tb cases are pulmonary, 20% are extrapulmonary and specifically abdominal TB accounts for approximately 10% of cases [4]. Tuberculosis can affect any intra-abdominal organ. The most frequent cite of abdominal tuberculosis is the ileocecal region. The other organs of the abdomen (liver, spleen, kidney, and pancreas) can also be affected by the disease [5]. Pancreatic tuberculosis, however, is a very rare type of TB that can mimic pancreatic carcinoma. The increase in reported cases of pancreatic TB in the last years can be attributed to improved imaging techniques such as EUS, which can obtain specimens from the pancreatic lesion [6]. EUS images can provide a first impression about the type of tumor, but biopsy is required for the final diagnosis. The clinical symptoms are variable, including abdominal pain, jaundice, fatigue, weight loss, fever, anorexia, peripheral lymphadenopathy and night sweats [7].
Tuberculosis is still a major health problem worldwide, with an estimated of 10 million individuals becoming ill in 2018 [7]. In the same year 1.5 million deaths were reported because of TB. In developing countries, TB is a constant problem [8]. The main factors responsible for the erection of the global TB epidemic are due to poverty, Human immunodeficiency Virus (HIV) infection, and drug resistance [8-9].
The most common type of Tuberculosis is pulmonary TB [7]. The bacilli reach the lungs of patient via droplet infection and if the immunity of the body fails to limit the infection, bacterial proliferation occurs inside the alveolar macrophages [7]. These bacilli migrate to other organs. Abdominal TB comprises about 10% of all TB cases which include the GI tract, peritoneum, lymph nodes or solid organs [5,7].
Gastrointestinal Tuberculosis can occur by ingestion of contaminated milk or meat. Infection can occur from adjacent organs or spread can occur via lymphatics. Pancreatic Tb is an extremely rare type of tuberculosis [7]. There are three forms of pancreatic TB that have been reported: miliary TB, spread from retroperitoneal lymph nodes to the pancreas and localized pancreatic TB [10]. The most common symptoms include weight loss (75%), anorexia (69%), fever (50%), jaundice (31%) and abdominal pain (25%). Pancreatic TB can mimic pancreatic carcinoma. The most common site of pancreatic TB is the head of the pancreas (~59%) following body (18%) and tail (13%). Usually, pancreatic TB presents with the form of mass (~80%) [10-11].
The imaging features of pancreatic Tb in CT are solitary parenchymal lesions (head>body), intra/peri-pancreatic collections, pancreatic duct dilatation, enlarged lymph nodes, granulomas in liver/spleen/omentum, ileocecal and peritoneal involvement and ascites. EUS findings include heterogeneous echotexture of the pancreas, and hypoechoic collections may be seen in some cases, peripancreatic lymphadenopathy and ascites [12].
Fine Needle Biopsy through EUS gives us the ability to obtain specimen from the pancreatic lesion, so the diagnosis is made soon enough to avoid further dilemmas. The diagnostic accuracy of EUS-FNA/FNB in pancreatic TB is difficult to determine due to the rarity of this entity [11]. It has been reported that the success rate of EUS-FNA/FNB for pancreatic TB ranging from 50-62% [10-11]. The pathology test confirms the diagnosis [13]. The common pathology findings are granulomas, inflammatory cells comprising neutrophils, lymphocytes and macrophages. The Ziehl-Neelsen stain for Acid-Fast Bacilli (AFB) showed positive results indicating presence of AFB [12-14].
The gold standard of treatment of Pancreatic TB includes anti-tubercular drugs. The duration of treatment is six months. The drugs administrated include Rifampicin (10mg/kg/day), Isoniazid (5mg/kg/day) Ethambutol (20mg/kg/day) and Pyrazinamide (30mg/kg/day). Conventional anti-tubercular treatment is adequate for Pancreatic tuberculosis that usually retreats completely [15]. Our patient received the standard quadruple therapy (Rifampicin, Isoniazid, Ethambutol, Pyrazinamide) and after 6 months he responded completely.
Conclusion
Pancreatic tuberculosis is a very rare form of abdominal TB, which still exists even in countries, like Greece, that was eliminated. This is a result of the migration from epidemic regions of TB. It is important to know that a pancreatic tumor is not always carcinoma. The symptoms are not specific and high levels of suspicion are needed to do the diagnosis. CT is important but the final diagnosis depends on pathology examination of the specimen we obtain through EUS-FNB. Conventional anti-tubercular treatment usually achieves complete response.
Conflict of interest
None to declare.
Funding
None.
Ethical Standards
Patient consent to publish this manuscript.
Conflict of interest
None to declare.
Acknowledgements
AK and IT gathered the data and wrote the manuscript, DK performed the EUS-FNB, DD reviewed the manuscript and MA performed the pathology test.
References
- Parenti DM, Steinberg W, Kang P. Infectious causes of acute pancreatitis. Pancreas. 1996 Nov;13(4):356-71. Doi: 10.1097/00006676-199611000-00005.
- Chuabio V, Bandoy J, Ong A, Te M 3rd, Maralit R. Pancreatic masses clinically diagnosed as tuberculosis: Case reports. SAGE Open Med Case Rep [Internet]. 2024 Jun; 12:2050313X241262192. Available from: https://pubmed.ncbi.nlm.nih.gov/38895655/ Doi: 10.1177/2050313X241262192.
- Selviani Tanic A, Dewi Tetanel LA, Xaverius Rinaldi F, Levina Polanit V, Ivano Kalaij AG, Julian Nelwan B. Pancreatic Tuberculosis Mimicking Pancreatic Tumor: A Case Report from Rural Area in Indonesia. Middle East J Dig Dis. 2024 Apr;16(2):119-121. Doi: 10.34172/mejdd.2024.379.
- Chaudhary P, Bhadana U, Arora MP. Pancreatic Tuberculosis. Indian J Surg. 2015 Dec;77(6):517–24. Doi:10.1007/s12262-015-1318-4.
- Panic N, Maetzel H, Bulajic M, Radovanovic M, Löhr J-M. Pancreatic tuberculosis: A systematic review of symptoms, diagnosis and treatment. United European Gastroenterol J. 2020 May;8(4):396-402. Doi:10.1177/2050640620902353.
- Abbaszadeh M, Rezai J, Hasibi M, Larry M, Ostovaneh MR, Javidanbardan S, et al. Pancreatic Tuberculosis in an Immunocompetent Patient: A Case Report and Review of Literature. Middle East J Dig Dis. 2017 Oct;9(4):239-41. Doi: 10.15171/mejdd.2017.80.
- Siddeek RAT, Gupta A, Singla T, Rajput D, Ahmed SS, Jeladharan R. Pancreatic tuberculosis mimicking as pancreatic malignancy: Surgeon’s dilemma. Indian J Pathol Microbiol. 2023 Jul-Sep;66(3):614-7. Doi: 10.4103/ijpm.ijpm_874_21.
- World Health Organization. Global tuberculosis report 2019 [Internet] [Accessed 2019 Oct 28]. Available from: https://www.who.int/tb/publications/global_report/en/
- World Health Organization. Global tuberculosis report 2020 [Internet] [Accessed 2021 Apr 5]. Available from: https://www.who.int/publications/i/item/9789240013131
- Ray S, Das K, Ghosh R. Isolated pancreatic and peripancreatic nodal tuberculosis: A single-centre experience. Trop Doct. 2021 Apr;51(2):203-9. Doi:10.1177/0049475520962941.
- Nagar AM, Raut AA, Morani AC, Sanghvi DA, Desai CS, Thapar VB. Pancreatic Tuberculosis: A Clinical and Imaging Review of 32 Cases. J Comput Assist Tomogr. 2009 Jan-Feb;33(1):136-41. Doi:10.1097/RCT.0b013e31816c82bc.
- Pramesh CS, Heroor AA, Gupta SG, Krishnamurthy S, Shukla PJ, Jagannath P, et al. Pancreatic tuberculosis: An elusive diagnosis. HPB (Oxford). 2003; 5:43–5. Doi:10.1080/13651820310000262.
- Saluja SS, Ray S, Pal S, Kukeraja M, Srivastava DN, Sahni P, et al. Hepatobiliary and pancreatic tuberculosis: A two-decade experience. BMC Surg [Internet]. 2007 Jun;7:10. Available from: https://pubmed.ncbi.nlm.nih.gov/17588265/ Doi:10.1186/1471-2482-7-10.
- Kumar PA, Singh G, Joseph JB, Swaminathan S, Venkatakrishnan L. Pancreatic Tuberculosis: A Puzzle for Physicians. A Rare Case and Review of Literature. J Clin Diagn Res [Internet]. 2016 Nov;10(11):PD29-PD31. Doi: 10.7860/JCDR/2016/22995.8896. Available from: https://pubmed.ncbi.nlm.nih.gov/28050442/
- K Bharat, C Vijayakumar, TP Elamurugan, Sudharsanan S, Sadasivan J. Primary Pancreatic Tuberculosis: A Rare Case Report. Adv Res Gastroentero Hepatol. 2019;13(2): 555858. Doi: 10.19080/ARGH.2019.13.555858